Obesity Skin Problems – Main Causes and Risks
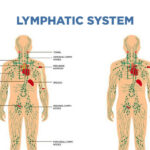
Several variables have been linked to obesity as a possible skin issue trigger. Hormonal shifts can bring on stretch marks and acanthosis nigricans (dark, velvety patches in the neck and body folds) is a condition that can occur as a result of skin stretching (striae). An increase in leg vein pressure can lead to fluid retention, leg edema, capillary rupture (capillaritis), varicose veins, dermatitis, and even ulceration.
Infections like intertrigo can develop when bacteria and fungi thrive in warm, dark places like body folds. Finally, the extra pressure on the foot could lead to corns and calluses. With a balanced diet and accompanying weight loss, many of these obesity skin problems will disappear.
Can obesity cause obesity skin problems?
Numerous obesity skin problems can cause general changes to the skin’s appearance 1,3 in people who are obese (considered to have a BMI of 30 or greater). A study conducted on American women in 2017 indicated that obesity severely damaged the skin’s barrier and moisturizing capabilities, leading to much more dryness and roughness than in nonobese women.
Facial redness, thought to be caused by the dilatation of local blood vessels in reaction to inflammation, was observed, as well as a decreased yellow coloring of the skin. On the other hand, changes in interleukin (IL)-6, leptin, adipokines, and insulin levels showed that scaliness and roughness were the result of systemic inflammation in conjunction with insulin resistance.
What are 5 diseases caused by obesity?
The Risk of Stroke and Heart Disease
The risk of developing high blood pressure and high cholesterol increases in proportion to the amount of extra weight a person carries. Both of these disorders increase the risk of developing cardiovascular disease or having a stroke.
The good news is that even a little amount of weight loss can make a significant difference in one’s risk of developing cardiovascular disease or suffering a stroke. It has been established that dropping any more pounds brings the risk level down even further.
Type 2 Diabetes
The majority of individuals who are diagnosed with type 2 diabetes are either overweight or obese. You can lower your chances of acquiring type 2 diabetes by engaging in greater physical activity, shedding excess pounds, maintaining a healthy diet, and obtaining sufficient rest.
If you have type 2 diabetes, controlling your blood sugar levels can be made easier by reducing your body fat percentage and increasing the amount of exercise you get. Your requirement for diabetes medication may also decrease if you engage in greater physical activity.
Gallbladder Disease
If you are overweight, you have a greater risk of developing gallbladder disease and gallstones. Ironically, the process of losing weight, and particularly losing weight quickly or losing a significant amount of weight, can increase the likelihood that you will develop gallstones. Gallstone formation is reduced in patients who lose weight at a rate of approximately one pound per week.
Osteoarthritis
The knee, the hip, or the back are the joints that are most frequently impacted by osteoarthritis, a condition that affects the joints. Carrying around additional weight puts additional pressure on these joints, which in turn causes the cartilage (tissue that cushions the joints) that typically protects them to wear away.
Losing weight can reduce the strain placed on joints like the knees, hips, and lower back, and it also has the potential to relieve osteoarthritis symptoms.
Sleep Apnea
The disease known as sleep apnea is a breathing disorder that is associated with being overweight. Snoring and momentary pauses in breathing while asleep are two symptoms that may be caused by sleep apnea in a person.
In addition to increasing the risk of cardiovascular disease and stroke, sleep apnea may also cause daytime tiredness. Losing weight is one of the most effective treatments for sleep apnea.
Why do obese people have scaly skin?
Obesity-related health issues, particularly obesity skin problems, are becoming more complex. The increase in stored fat associated with obesity can impact skin physiology and is implicated in a spectrum of dermatologic conditions. The ability of obese skin to handle transepidermal water loss is impaired.
Fat reserves enhance transepidermal water loss, causing dryness and delayed skin healing. Obese people may sweat profusely (hyperhidrosis) when overheated or active due to their extensive subcutaneous fat layers. Hyperhidrosis causes skin injury. Moisture trapped in skin folds, friction as body folds rub together, and inadequately perfused adipose tissue can undermine skin integrity and postpone healing.
Complex obesity skin problems and the potentially fatal implications of skin breakdown in obese people make it vital that they have a full skin assessment upon admission to any health service. This is step one in identifying uncommon obesity skin problems.
A superficial evaluation isn’t enough. A good bodily exam may require two or more people. All skin folds and panniculus should be inspected for erythematous, fungal, damp denuded regions, or pressure injuries.
How does obesity cause keratosis pilaris?
Keratosis pilaris is an obesity skin problem that affects roughly 16% of the population and is characterized by palpable sterile papules and/or pustules. The posterior aspect of the upper arms, anterior thighs, face, and buttocks are the most usually affected areas; however, keratosis pilaris lesions can develop anywhere except the soles and palms.
Despite the fact that keratosis pilaris is a harmless illness, these lesions are associated with severe cosmetic comorbidity, with 69% of patients feeling unhappiness as a result of their rash.
This is especially concerning given that these lesions are most typically found in adolescent females, many of whom may already be struggling with body image concerns. Patients with face involvement, substantially inflamed, red lesions, and those who already have a low body image are more likely to experience major distress from this illness.
Although the exact cause of keratosis pilaris is not understood, researchers have discovered a correlation between this skin condition and a variety of other health issues. Keratosis pilaris is linked to a number of risk factors, the most notable of which are obesity, dry skin, and atopic diathesis.
This condition, which is commonly associated with having dry skin, tends to become worse throughout the winter months. It is important to highlight the fact that it is considered that hyperinsulinemia is the root reason for its relationship with obesity.
It is believed that an increase in the amount of insulin that is circulating in the blood causes concomitant increases in the synthesis of androgen, which leads to follicular keratinization, which ultimately results in the formation of keratosis pilaris.
Because insulin-dependent individuals have a higher risk of developing lesions at the sites where they inject insulin, this physiologic alteration is of clinical significance. Keratosis pilaris is often diagnosed on clinical grounds; nevertheless, it is vital for doctors to separate keratosis pilaris from other, more problematic lesions. Keratosis pilaris is generally diagnosed on clinical grounds.
Sources:
https://www.dermatologyadvisor.com/home/topics/general-dermatology/effects-of-obesity-on-skin/
https://skinsight.com/disease-groups/skin-problems-related-to-obesity/
https://www.webmd.com/diet/obesity/obesity-health-risks