What Is the Difference Between Osteoporosis and Osteoarthritis?
In the world of biology and medicine, we know that the prefix “osteo-” refers to bones. But with so many developments and complications around bone health, it may be easy to get confused about what the difference is between two common bone-related conditions. We are talking about osteoporosis vs osteoarthritis.
In the United States, it is said that there are over 44 million people with osteoporosis, with some saying the figure is as high as 54 million. As for osteoarthritis, there are over 32.5 million US adults with the condition. But how similar are the two, what are the key differences, and what are some ways to manage these conditions? Read on to find out more.
- 1 Osteoporosis vs osteoarthritis: the key differences
- 2 Can you have both osteoporosis and osteoarthritis?
- 3 What are the 5 symptoms of osteoporosis?
- 4 What are the 4 stages of osteoarthritis?
- 5 Which is worse osteoarthritis or osteoporosis?
- 6 In conclusion: means of rehabilitating osteoporosis and osteoarthritis
Osteoporosis vs osteoarthritis: the key differences
We kick off our discussion with a comparison of osteoporosis vs osteoarthritis. In this section, we will look at what each medical condition is, their signs and symptoms, causes, complications, and treatments. Let’s dive in.
What it is
When it comes to osteoporosis (OP), we have a long-term (chronic) medical condition that is characterized by fragile and weak bones. “Osteoporosis” refers to “porous bones”. As such, these bones are much more prone to easier fracturing and breakages. Some of the most commonly affected areas are the hips, wrists, and the spine. OP develops slowly with few, if any, symptoms and limited pain.
However, although not noticeable to the eye, OP means that bone mass and density become limited, and therefore, bone strength is affected making them weaker. Consequently, OP occurs when the body either loses too much bone, makes too little bone, or both. Viewed from another perspective, OP develops when the body reabsorbs more bone tissue but does not produce enough to replace it.
As for osteoarthritis (OA), also called degenerative joint disease (DJD), degenerative arthritis, or wear-and-tear arthritis, this goes beyond bone density and mass but rather affects the entire joint in the human body. This includes physical factors such as the bone, cartilage, ligaments and tendons, fat, and the tissues which line the joint. OA – also a chronic condition – can result in a degradation of cartilage, it can change bone shape, it can cause bony changes, deform the joint, and cause inflammation.
Although it was commonly referred to as a “wear-and-tear” condition of the joints in the past, today, researchers do not know what triggers the breakdown of joint tissues. It is the most common type of arthritis in this family of ailments. Although OA can occur in practically any joint in the body, some of the most commonly affected areas are the hands, fingers, shoulder, spine (neck or lower back), hips, and knees. It happens when cartilage breaks down and a situation of bone rubbing against bone occurs.
Signs and symptoms
We will now explore the common signs and symptoms related to osteoporosis vs osteoarthritis.
With OP, it must be noted that there are few, if any, symptoms of this condition. This is why it is often referred to as a “silent disease”. However, a patient with it may suffer from fragility-related fractures as a result of a mild impact. Other issues can include height-loss over time, receding gums, a curved spinal shape, lower back pain, shortness of breath, weakened grip strength, weak/brittle nails, and tiny cracks in the bones, known as stress fractures.
OA, on the other hand, is characterized by a series of symptoms. These include joint pain during movement as well as joint stiffness or tenderness. Other signs include loss of flexibility, a grating sensation or popping/crackling when moving your joints (crepitus), bone spurs, swelling, muscle weakness around the joint, feeling as though the joint is loose or unstable, changes in joint shape, and/or morning stiffness or stiffness during cold or damp weather.
Causes
Being diagnosed with OP is associated with a variety of medical and non-medical causes. Some examples include taking high-dose steroid tablets for a period longer than three months; inflammatory, hormone, or malabsorption conditions; genetics and family history; eating disorders and low body mass index; infrequent exercise; heavy drinking and smoking; autoimmune disorders; neurological disorders; blood and bone marrow disorders; mental illness; endocrine/hormonal disorders; AIDS/HIV; Chronic obstructive pulmonary disease (COPD); chronic kidney disease; liver disease; organ transplants; polio and post-polio syndrome; diet, including malnutrition; scoliosis; weight loss; and pregnancy and lactation associated osteoporosis (PLO); and early menopause, among others.
Some of the associated causes of OA may include progressing towards an advanced age; gender (it is more common and severe in women); being overweight/obese; a history of injury or surgery to a joint; joint overuse; incorrect joint formation and joint abnormalities; genetics and family history; and poor posture.
Complications
We will now briefly explore the complications related to osteoporosis vs osteoarthritis. With OP, we are looking at debilitation in terms of performing daily activities as well as bone pain. Furthermore, patients may have more frequent fractures, and with age, these take longer to heal. As such, patients can experience ongoing pain and possibly loss of independent living.
With OA, some of the associated complications include but are not limited to poor sleep, weight gain due to limited mobility or pain, bone death, tendon and ligament erosion, hairline fractures, bleeding near the joints, etc.
Treatment
Although OP cannot be completely reversed and it is not considered curable, it is possible to make some lifestyle adjustments to manage the condition and improve the situation of bone loss. Examples of steps you can take to manage your health better include avoiding smoking and alcohol intake; doing regular weight, strength, and balance training exercises; eating healthy and maintaining a healthy weight; ensuring you take fall prevention measures; certain medication, etc.
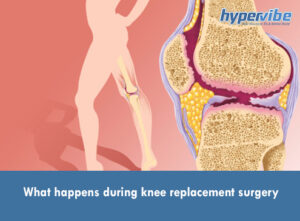
As for OA, there are mild and severe ways to attempt to manage the condition, even though it too cannot be cured or reversed. From lifestyle changes, which include healthy eating and weight loss, intermittent hot and cold packs, exercise, supportive devices, physical therapy, patients can also take medication such as oral analgesics and intra-articular injection therapies, vitamins and supplements, and as a final resort, there is surgery.
Can you have both osteoporosis and osteoarthritis?
When it comes to osteoporosis vs osteoarthritis, at first glance, they do share some common features particularly with the relationship between bone mass and density. However, they have key differences which must be considered. However, although they are different conditions, it is possible for a patient to have both at the same time.
What are the 5 symptoms of osteoporosis?
As mentioned above, there are few if any symptoms of OP. However, some of the most frequently encountered ones include: higher levels of fragility-related fractures; height loss; receding gums; a curved/stooped spine shape, and lower back pain.
What are the 4 stages of osteoarthritis?
The four primary stages of OA include minor, mild, moderate, and severe. With the minor stage, there is minor wear and tear in the joints; the mild stage is characterized by stiffness after sedentary periods and noticeable bone spurs. Meanwhile, with the moderate stage, there is more pronounced cartilage erosion and joint inflammation; while the severe stage is characterized by severe levels of pain.
Which is worse osteoarthritis or osteoporosis?
According to research, both conditions – osteoporosis vs osteoarthritis – have different stages and this makes it difficult to compare the two because every patient will be at a different stage of the condition’s development. However, what can be said is that OP is considered a “worse” condition, particularly if severe, owing to the higher risk of fractures, which may take a long time to heal.
In conclusion: means of rehabilitating osteoporosis and osteoarthritis
What becomes apparent when looking at osteoporosis vs osteoarthritis is the fact that both conditions require significant lifestyle changes such as exercise that is low-impact on the joints and dietary changes. One of the ways of rehabilitating these conditions or easing the symptoms is through whole-body vibration by using a vibration plate. This is a gentle yet impactful way of helping to strengthen the muscles and bones, while relieving some of the symptoms.
Resources:
http://www.cdc.gov/arthritis/basics/osteoarthritis.htm#:~:text=Osteoarthritis%20(OA)%20is%20the%20most,underlying%20bone%20begins%20to%20change.
http://www.niams.nih.gov/health-topics/osteoarthritis
http://www.healthline.com/health/osteoarthritis/natural-home-remedies#next-steps
http://www.nhs.uk/conditions/osteoarthritis/