Sudden Lower back pain when bending over can stem from various causes, including
Addressing this pain often involves rest, physical therapy, and sometimes medication.
It seems to always happen as if out of nowhere. You lean forward to pick up a sock, load the dishwasher, or grab a dropped pen, and there’s a “snap.” What comes next is a bolt of pain that radiates through your lower back, stealing your breath, buckling your knees, and sending your brain into panic mode.
It is believed that 4 in 5 adults will experience lower back pain at least once in their lives, and most episodes will settle within six weeks.
It is one of the most common, and most frustrating, experiences reported in doctor’s offices and orthopedic injury centers.
One useful recommendation when this occurs is to learn how to use your core for stability and move with the right alignment. There is no better way to improve these proprioceptive skills than with Whole Body Vibration.





Here’s a breakdown of the most common signs to look out for:
This type of pain is typically linked to a muscle strain or spasm, often caused by lifting something heavy, twisting incorrectly, or moving suddenly.
It may feel like a stabbing or jolting pain that catches you off guard, especially when bending over.
According to Continuous Motion Physical Therapy, this pain can even occur during gentle movements and should be addressed promptly with rest and ice.
A dull ache across the lower back is often the result of muscle fatigue, overuse, or poor posture—especially after long periods of sitting or standing.
It may not feel intense but can gradually worsen if the root cause isn’t corrected.
If you experience lower back pain that travels down one leg, it could be a sign of nerve irritation or compression, often from a herniated disc or sciatica.
This symptom may come with numbness, tingling, or weakness in the leg and should be evaluated by a healthcare professional.
Struggling to bend, twist, or stand up straight? A limited range of motion can indicate tight muscles, inflammation, or a mechanical issue within the spine.
You might feel stiff or blocked when trying to perform everyday movements.
Muscle spasms often occur as a protective response when the body detects an injury.
They can feel like tight, uncontrollable contractions in the lower back, making movement painful or difficult.
Spasms are especially common in the first 24–48 hours following a strain and are often treated with a combination of ice, rest, and gentle movement.
Ongoing stiffness, especially in the morning or after prolonged sitting, may point to inflammatory conditions like ankylosing spondylitis or arthritis.
This symptom usually improves with movement and gentle stretching.





There are a wide array of reasons that your back can “give out.” Common among most of them is a loss of the normal curvature in the low back (the lordosis), often from poor posture and prolonged sitting.
Each time you bend over, there is a degree of compression that occurs, slowly increasing pressure on the front of the spine.
This can cause stress on ligaments, joints, and, the usual suspect in extreme cases, the lumbar discs.
Intradiscal pressure roughly doubles compared with upright standing normally, so imagine how much stronger it can be when it’s increased.
Nonetheless, in most cases of low back pain, there are several likely pain sources:
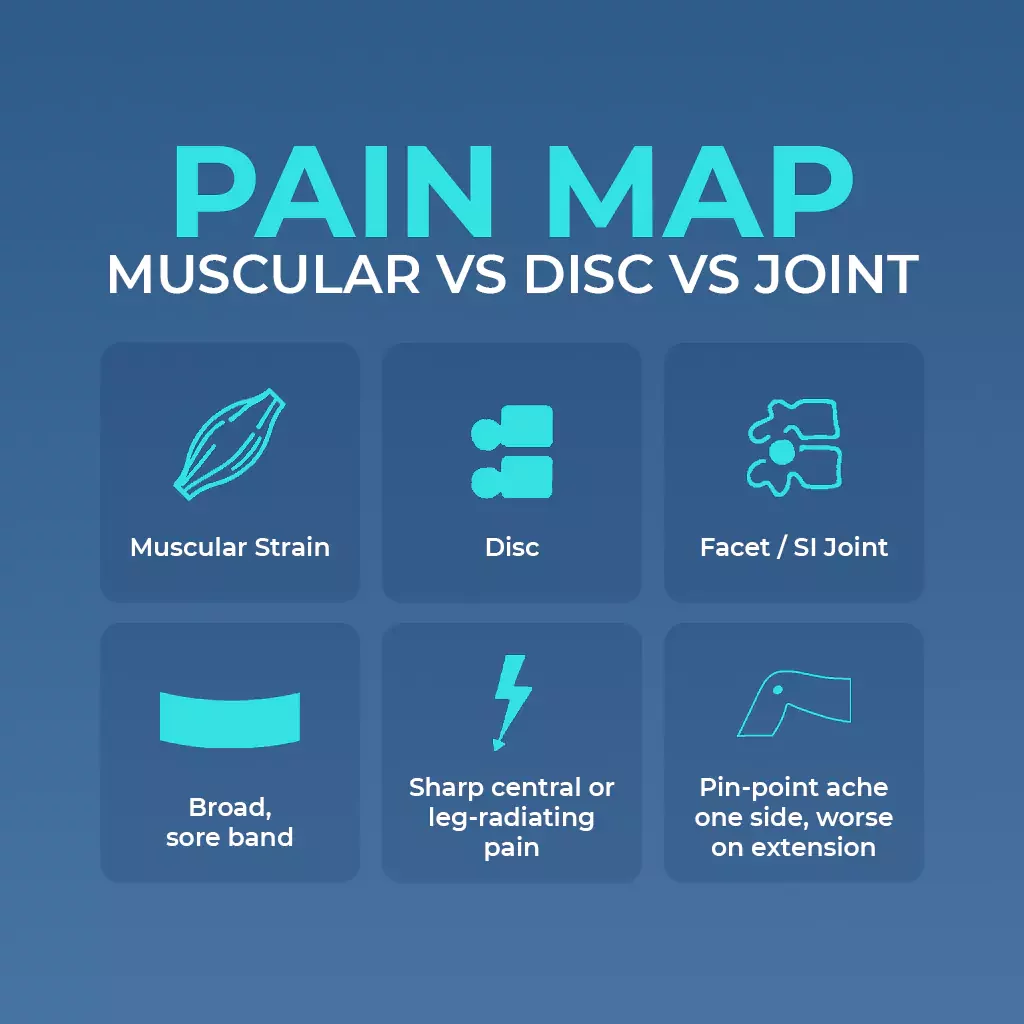
infographic on the pain map of lower back pain based on the cause
An intervertebral disc has a tough outer ring (annulus fibrosus) and a gel-like core (nucleus pulposus).
A “slipped” or herniated disc occurs when the nucleus ruptures through a torn annulus and bulges toward the spinal canal.
When this occurs, there can be increased pressure on neighboring nerves and chemical interactions that cause inflammation and pain.
Common injuries and symptom patterns:
All of these can accelerate annular degeneration and raise herniation risk.
Quick self-check:
Your doctor may order an MRI (or CT if MRI is unavailable) when radicular pain or numbness lasts more than 6 weeks, if significant neurological deficits appear (loss of muscle function or feeling), or if any other possible red flag is present.
A plain X-ray is reserved for suspected fracture or severe osteoarthritis, while an EMG helps confirm nerve-root damage if imaging is equivocal.
The presence of any red flag warrants same-day imaging and specialist referral.

Infographic on different ways to treat lower back pain
Here are expert-backed strategies on how to treat lower back pain safely and effectively:
When lower back pain starts suddenly, especially from a strain or minor injury, rest and apply ice packs during the first 24 to 48 hours.
Ice helps reduce inflammation, swelling, and sharp pain.
Avoid prolonged bed rest; short rest periods combined with gentle movement are more effective for healing.
After the initial inflammation subsides, switch to heat therapy.
Applying a warm compress or using a heating pad can help relax tense muscles, increase blood flow, and ease stiffness in the lower back.
Incorporating light stretches can help relieve pressure and improve flexibility.
Some effective stretches for lower back pain include:
Always move slowly and stop if pain increases.
Once the pain begins to improve, focus on core strengthening exercises.
Strong abdominal and back muscles offer better support to the spine and reduce the risk of future pain.
A few gentle exercises include:
These exercises are often part of a guided physical therapy plan on how to treat lower back pain holistically.
Poor posture can strain your back muscles.
Practice keeping a neutral spine:
Improper lifting is a common cause of sudden lower back pain.
Follow these steps:
A licensed physical therapist can assess your condition and develop a personalized plan.
They’ll guide you through safe stretches, strength training, posture correction, and daily movement patterns that prevent pain from returning.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help manage inflammation and reduce pain during the early stages.
Use them as directed and consult your doctor if the pain persists.
If your lower back pain doesn’t improve with home care or becomes worse, consult a doctor or physical therapist.
Conditions like herniated discs, muscle spasms, or nerve impingements require professional evaluation and targeted treatment options, which may include advanced therapies like spinal injections or chiropractic care.





Three controlled trials say yes—Whole Body Vibration can help when dosed carefully:
Safe home settings for Whole Body Vibration: stand with soft knees at 8-12 Hz, low G-force, 30-60 s to start, and progress to 3-5 minutes. Then, repeat for 2 sets.
Lower Back Pain – Pin
Rest 30s between moves; stop if you have leg numbness, loss of strength, or if pain increases.
To maintain long-term prevention, use a hip hinge when bending.
Practice with feet shoulder-width and spine neutral.
Hinge at the hips while the chest stays up and the core is engaged. Keep weight through the heels when possible.
Core-strength WBV routine that helps with core strength—plank progressions (use mat on plate):
Train 3× a week, and advance by adding 10 s every fortnight.
Having strong transverse abdominis and multifidus muscles cuts disc shear during daily tasks significantly.
Lifestyle Tips:
Seek urgent medical care if any of the following appear:

elderly woman on hypervibe vibration plate with the headline Do vibration plates work for back pain
These red flags can signal cauda equina syndrome, disc infection, or other emergencies requiring prompt imaging and treatment.
Most herniated discs settle with conservative care in 6–12 weeks; studies show 85-90% of patients are pain-free by three months.
Pain often begins easing in the first 2–6 weeks, though complete disc resorption can take up to six months.
Persistent deficits beyond 12 weeks need specialist review.
Extended bed rest is counterproductive for disc pain.
Clinical guidelines favor staying active; if pain is intense, limit rest to ≤48 hours, then resume gentle movement.
Early mobilization reduces pain and disability more effectively than lying down for days.
Yes—once acute pain has settled and a clinician clears you—begin with light, pain-free loads, core-bracing drills, and strict neutral-spine technique.
Avoid heavy axial lifts such as deadlifts and back squats until you regain full, symptom-free range and baseline strength.
Evidence is weak: inversion tables may give brief pain relief or delay surgery in select disc cases, but systematic reviews find no lasting benefit for most back-pain patients.
They’re contraindicated in glaucoma, uncontrolled hypertension, or heart disease, so consult a doctor first.

Here’s how we use a vibration plate for weight loss...

Many people, especially beginners, notice an itchy or tingling “pins-and-needles”...

Yes, Vibration Plates or Whole Body Vibration (WBV) platforms, promote...
Are vibration machines bad for you? Yes, if used incorrectly....

Most people get the best results using a vibration plate...